Overview:
Osgood–Schlatters disease (OSD) is one of the most common causes of knee pain in active adolescents. A large number of you would have had it in the past and a large number of your children may experience it. OSD occurs due to the repetitive force of the Quadriceps pulling on the patella tendon as in attaches to the tibial tuberosity. It more commonly affects boys (aged 10–15), however can also been seen in girls (aged 8-14).
Cause:
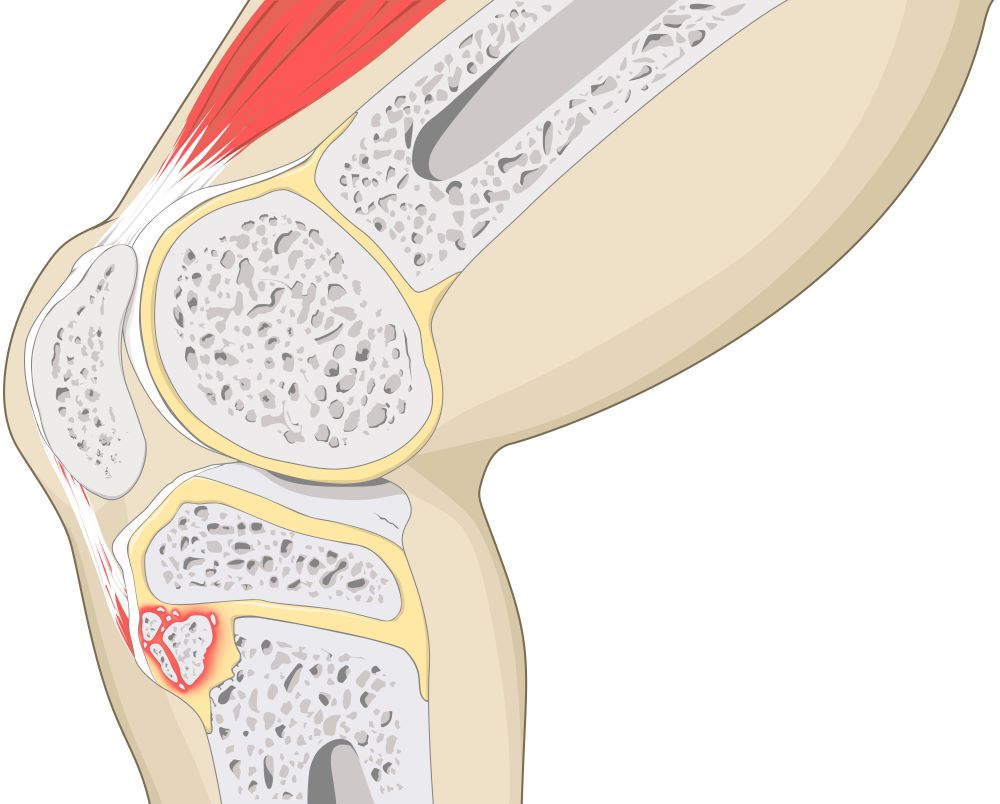
During adolescents, bone goes through several stages of growth. During the second phase of growth known as apophysis, the bone is unable to withstand high forces. The strong and repetitive muscle contractions from the Quadriceps muscle places a high force on the tibial tuberosity; resulting in mircofractures – or OSD. Activities that involve running, jumping (such as basketball, running, volleyball, gymnastics) and direct contact (kneeling) exacerbate symtpoms.
Symptoms:
OSD symptoms have a gradual onset with mild intermittent pain developing to severe and continuous pain accompanied by limping. Swelling and enlargement of the tibial tuberosity at the patella tendon’s insertion side can also be seen.
Prognosis/outcome
The overall prognosis for OSD is usually self-limited. Complete recovery is expected when the tibial growth plate closes within 2 years, providing a good long-term outcome for the majority of patients. Most patients are able to return to full activity within 2 to 3 weeks. In some cases complications can occur: discomfort in kneeling, residual bony deformity and painful ossicles (small bone fragments) in the patellar tendon- all leading to continuing activity restrictions.
Intervention (treatment):
90% of patients respond well to conservative treatment:
- Physiotherapy modalities
- analgesic medication and ice for pain relief
- rest from painful activity/ activity modification followed by:
- stretching and strengthening exercises once symptoms are controlled
OSD can lead to surgery in rare cases for those who remain symptomatic despite conservative measures.
Please call Holistic Physio Fitness on 9999 6666 to discuss further.
Bibliography
Cakmak, et al. (2014). Long-term outcome of Osgood-Schlatter disease: not always favorable. Rheumatology International, Vol 34 (1) 135-136.
Hanada, et al. (2012). Relationship between the clinical findings and radiographic severity in Osgood–Schlatter disease. Open Access Journal of Sports Medicine, 17-20.
Kaya et al. (2013). Long-term functional and sonographic outcomes in Osgood–Schlatter disease. Knee Surg Sports Traumatol Arthrosc, 21: 1131–1139.
Purushottam et al. (2007). Osgood Schlatter syndrome. Current Opinion in Pediatrics, Vol 19 (1) 44-50.
Wall et al. (1998). Osgood-schlatter disease: practical treatment for a self-limiting condition. Phys Sportsmed, 29-34.

